Let’s start with a very short story about me and a typical patient.
“Hi, my name is Andrew and I am your physiotherapist. I’ve never met you before but considering you’re in a hospital, I’m expecting you to completely trust me within the next few minutes and reveal deep dark secrets about your physical, mental and sexual health. So let’s get cracking…”
Now, let me ask you this question. How likely would you be to trust an absolute stranger dressed like a pool cleaner, separated from other patients (some might even be your neighbour) by only wafer thin curtains. These paper towels offer absolutely no soundproofing, which results in anyone within a five metre range hearing whether you have been having morning erections or not? My guess is - not very likely. This scenario sets the stage for a deeper conversation about the intersection of food, exercise, and building trust in therapy.
We have a tough job and encounter a variety of patients every day, each with their unique stories and challenges. The reality of healthcare is that medical professionals face immense pressure: tight schedules, emotional patients, and the urgent need to alleviate pain quickly. When a patient finally steps into the clinic after a long wait, they often bring with them a tide of frustration, anxiety, and unmet expectations. They might express their woes, from sleepless nights to strained relationships, all while you’re trying to gather information and formulate an effective treatment plan in less than 30 minutes.
This environment can lead to what I call, Therapist Anxiety Syndrome (TAS), where the rush to diagnose and treat can overshadow the essential elements of active listening and empathy. Furthermore, research has shown a significant correlation between patient trust and adherence to prescribed rehabilitation programs [1][2]. If patients feel unheard, their trust diminishes, which can negatively impact their adherence to treatment plans [3].
Consider this scenario: Your patient arrives five minutes late for a 30-minute appointment. Just before their arrival, the administration staff informs you that your previously scheduled admin time has been converted into a new patient appointment. The patient starts by expressing their frustration about the long waiting times and mentions that they were delayed due to a full car park. Take a moment to reflect on this situation. How are you feeling right now? On a scale of 1-10 on the ‘TAS’ scale (a made-up scale, but you get the idea), where would you rate your emotional state? If your score is above 5, it’s likely that active listening and empathy may not be your top priorities at this moment leading to a significant conundrum. On one hand, TAS will push you towards gathering essential information from the patient quickly. This could involve interrupting the patient as well as using an uninviting tone and body language. On the other hand, you also understand that extensive research shows that effective communication and strong therapeutic relationships are crucial in musculoskeletal care [4][5][6].
Before we try and address this issue, let’s briefly explore the research on therapy adherence. Adherence to rehabilitation can vary significantly, with rates reaching up to 90% but dropping as low as 14% [7][8][9]. Interestingly, providing patients with more information can lead to less favourable outcomes [10]. When we take a closer look, it appears that individuals start off quite motivated during rehabilitation programs, with adherence rates around 70% in the first six weeks. However, this drops to as low as 20% over longer periods (more than 3 months) [11].
As Professor Angela Duckworth, psychologist and author, notes, “Enthusiasm is common, endurance is rare.” [12].
Additionally, it’s important to note that in the UK, approximately one in three adults (30%) are deemed physically inactive, engaging in less than 30 minutes of activity per week based on national statistics. Yes, that's just 30 minutes weekly. Moreover, social deprivation impacts physical activity levels, reducing participation from 73% to 57% in more socio-economically deprived areas.
These statistics suggest that a large segment of the UK population is not engaging in sufficient physical activity, and maintaining long-term commitment to rehabilitation proves challenging for many. Despite this, therapists often feel pressured (TAS) to distribute numerous exercise sheets for patients to follow multiple times a day, hoping that something resonates.
But what if the solution to this dilemma lies not just in clinical techniques, but also in the way we understand and relate to our patients? I want to propose a slightly unusual analogy using food - specifically Italian cuisine versus Indian cuisine - to illustrate how we can tailor our exercise prescriptions to suit individual patients.
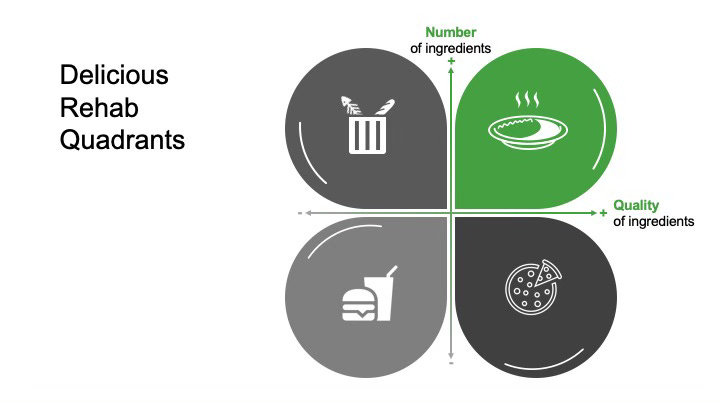
If you've been fortunate enough to visit Italy, you’ll notice that Italians often use a select few high-quality ingredients in their cuisine. The emphasis is on quality; they use the freshest pasta, cooked perfectly with just the right amount of salt, paired with the ripest tomato sauce and topped with the most flavourful local cheeses (don’t even get them started on parmesan!). In slight contrast, good Indian cuisine requires a variety of high-quality ingredients that are layered over time to create a rich culinary experience. Refer to [Fig 1] for a visual representation of this concept. In essence, both Italian and Indian cuisines depend on good quality ingredients to shine.
Fig 1. Delicious Rehab Quadrants
Italian food patients are those who typically express a lack of physical activity and a disinterest in exercise or multiple exercises (gym), often preferring just one type of activity like running or walking. Recognising that a patient embodies the ‘Italian food’ mentality can help you determine the appropriate amount of time needed for their exercise prescription after your assessment, alleviating the pressure to provide a multitude of activities and thereby reducing TAS.
Consider a simple interaction with an Italian food patient: a patient arrives with shoulder pain. You have a 30-minute window to assess and prescribe treatment. Assuming they’re punctual, they begin explaining their shoulder issue and you quickly identify them as an Italian food patient. However, you also realise that their neck may be contributing to the shoulder problem. This discovery extends your questioning, and before you know it, 15 minutes have passed without a definitive conclusion. As the clock ticks down, you feel the pressure to establish a diagnosis and address multiple treatment targets such as pain management, range of motion, strength, confidence, and proprioception. Welcome to TAS. These feelings can cloud your judgment and prompt you to rush through the subjective assessment. But remember, since they are an Italian food patient, you don’t need to overwhelm them with numerous exercises.
Instead, focus on identifying the main priority for the patient. A simple contracting question at the beginning can be very effective: “We have 30 minutes; what would you like to achieve in today’s session?” Often, they may just need reassurance about their issue. Quality reassurance is critical here. While the urge to hand them an information leaflet on frozen shoulder filled with exercises and detailed explanations is strong, remember that less can be more. They can leave with the necessary information and a follow-up appointment scheduled. At the next visit, you can suggest a maximum of 1-3 exercises based on their priorities discussed during the follow-up.
Key steps in this interaction include:
1. Contracting to set clear expectations.
2. Managing the urge to provide excessive information or rush through the assessment.
3. Delivering a low-volume, high-quality management approach; akin to Italian cuisine.
Now, let's transition from Rome to Mumbai. A patient walks in with hip pain, sporting gear from a well-known gym brand. They tell you they work out for 60 minutes, 3-4 times a week, completing around 6-7 exercises per session, and have maintained this routine for the past three years. This patient embodies the ‘Indian food’ mentality, and just like the previous scenario, TAS surfaces after 15 minutes. Their primary concern revolves around maintaining their gym routine, which they find essential for their mental well-being. This is something you pinpoint during the contracting phase. This desire to continue training while injured is common among Indian food patients and contributes to TAS, as there’s pressure to address multiple exercises in a short space of time. However, understanding that they are comfortable with various exercises and equipment allows you to navigate their gym routine effectively. In the wrap-up phase of your appointment, you can quickly adjust or modify their routine with minimal explanation. This saves you time, keeping the patient satisfied while they await their next appointment. The follow up session can then focus on specific rehabilitation exercises tailored to their needs.
These patient types will often (depending on the rehabilitation phase) handle more rehab exercises because their body is accustomed to training, which can be slotted into their regular gym routine to improve adherence.
In healthcare and life, individuals exist on spectrums, and this metaphor can be adjusted according to your own knowledge, time constraints and of course the stage of rehab the patient is currently in. It will obviously vary between patients and still requires good clinical reasoning. It hopefully serves as a time and stress management strategy for therapists, encouraging a moment of pause to avoid overwhelming patients with excessive information or exercises in the name of quality care. Remember, it's not about overloading patients with rehab; it’s about delivering high-quality, effective rehabilitation.
Grazie!
References
[1] Jack K, McLean SM, Moffett JK, Gardiner E. Barriers to treatment adherence in physiotherapy outpatient clinics: a systematic review. Man Ther. 2010 Jun;15(3):220-8. doi: 10.1016/j.math.2009.12.004. Epub 2010 Feb 16. PMID: 20163979; PMCID: PMC2923776.
https://pubmed.ncbi.nlm.nih.gov/20163979/
[2]Jordan JL, Holden MA, Mason EE, Foster NE. Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults. Cochrane Database Syst Rev. 2010 Jan 20;2010(1):CD005956. doi: 10.1002/14651858.CD005956.pub2. PMID: 20091582; PMCID: PMC6769154.
https://pubmed.ncbi.nlm.nih.gov/20091582/
[3] Safran DG, Taira DA, Rogers WH, Kosinski M, Ware JE, Tarlov AR. Linking primary care performance to outcomes of care. J Fam Pract. 1998 Sep;47(3):213-20. PMID: 9752374.
https://pubmed.ncbi.nlm.nih.gov/9752374/
[4] Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009 Aug;47(8):826-34. doi: 10.1097/MLR.0b013e31819a5acc. PMID: 19584762; PMCID: PMC2728700.
https://pubmed.ncbi.nlm.nih.gov/19584762/
[5] O'Keeffe M, Cullinane P, Hurley J, Leahy I, Bunzli S, O'Sullivan PB, O'Sullivan K. What Influences Patient-Therapist Interactions in Musculoskeletal Physical Therapy? Qualitative Systematic Review and Meta-Synthesis. Phys Ther. 2016 May;96(5):609-22. doi: 10.2522/ptj.20150240. Epub 2015 Oct 1. PMID: 26427530.
https://pubmed.ncbi.nlm.nih.gov/26427530/
[6] Lin I, Wiles L, Waller R, Goucke R, Nagree Y, Gibberd M, Straker L, Maher CG, O'Sullivan PPB. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med. 2020 Jan;54(2):79-86. doi: 10.1136/bjsports-2018-099878. Epub 2019 Mar 2. PMID: 30826805.
https://pubmed.ncbi.nlm.nih.gov/30826805/
[7] MCLEAN, S., BURTON, M., BRADLEY, L. and LITTLEWOOD, C. (2010). Interventions for enhancing adherence with physiotherapy: a systematic review. Manual Therapy, 15 (6), 514-521. https://www.sciencedirect.com/science/article/abs/pii/S1356689X10000871?via%3Dihub
[8] Bassett S.F. (2003). The Assessment of Patient Adherence to Physiotherapy Rehabilitation. New Zealand Journal of Physiotherapy 31(2): 60-66.
[9] Martin LR, Williams SL, Haskard KB, Dimatteo MR. The challenge of patient adherence. Ther Clin Risk Manag. 2005 Sep;1(3):189-99. PMID: 18360559; PMCID: PMC1661624
https://pubmed.ncbi.nlm.nih.gov/18360559/
[10] Sluijs E M, van der Zee J and Kok G J (1993b): Differences between physical therapists in attention paid to patient education. Physiotherapy Theory and Practice 9: 103-117.
[11] Schneiders A G, Zusman M and Singer K P (1998): Exercise therapy compliance in low back pain patients. Manual Therapy 3: 147-152.
https://www.sciencedirect.com/science/article/abs/pii/S1356689X98800052
[12] Duckworth, A. (2016). Grit: The power of passion and perseverance. Scribner/Simon & Schuster












What are fantastic analogy absolutely loved it
I read a piece on multi objective optimisation and this relies on underdatanding the trade offs out patient are making which in turn we should appreciate. I love more flavours of practice and it's application. An analogy is much the same. So yes I imagine I will in the right context. Thank you so much for this.