The devastating U-turn in July/August 2023 by NHSE WTE (NHS England Workforce, Training and Education - formerly HEE), who pulled the plug on the planned First Contact Practitioner (FCP) register has left thousands of FCPs in limbo. I have skin in the game and, like many others who were in training at the time, am left feeling demoralised, bemused and a little bit angry.
How it was Supposed to Work
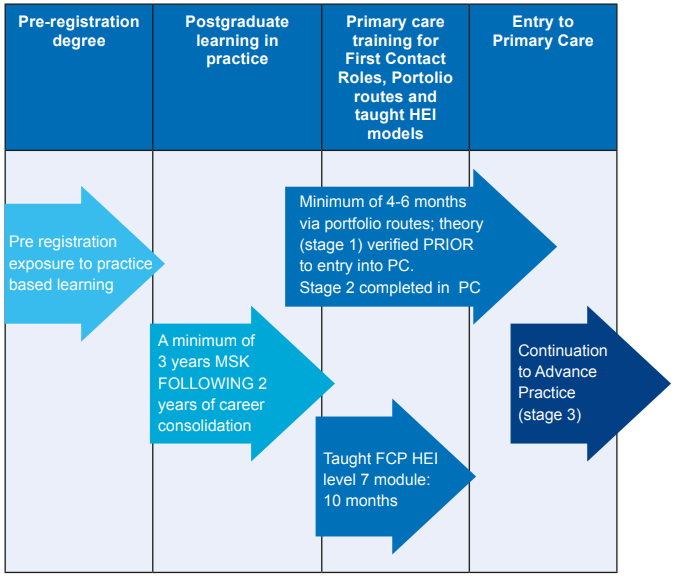
The FCPs in Primary Care Roadmap to Practice [1] was published in July 2021. It was developed by Health Education England now rebranded to National Health Service England after HEE merged with NHS England in 2023. It was a very big multi-organisational, group project combining patient and professional input. It is built on the 2018 MSK Core Capability Framework for FCPs [2]. Organisations that are members of the Arthritis and MSK Alliance (ARMA) were all involved in the project.
The roadmap defined the FCP role, training and educational pathway and it explained how to build a portfolio of evidence. It was designed to support and provide governance and link to NHSE Centre for Advancing Practice. FCPs were going to be registered at the Centre for Advanced Practice and registrants would receive a digital badge as part of this recognition.
For illustrative purposes this was how it looked [1]:
The Bad News
The roadmap was up and running until July/August 2023. Regretfully news of significant changes to it was badly communicated. NHSE failed to provide any sort of national announcement that the portfolio route was being scrapped. I will unpack the reasons later on in this article. For now it's useful to know what else was happening in the literature just prior to these changes.
One year prior to the U-turn, in September 2022 ARMA published the UK MSK Advanced Practice Standards Framework [3]. Its aim was to reduce unwarranted variation in education and practice at advanced practice level.
It used evidence from Noblet et al [4] to help inform the development of these standards. In Noblet et al they had called for accreditation of Advanced Practice. Its survey of the landscape described the FCP role as defragmenting advanced practice. It also recommended the FCP and Advanced Practice training take place through Higher Education Institutes (HEIs).
At the time of this study FCP was a new role and is mentioned as such. It goes on to say that FCP core capabilities and its acceptance in the community had not been investigated. It used a panel of experts to scrutinise the landscape.
The study concluded that urgent clarity and transparency of the title of Advanced Practice was required for patient safety. It also called for the Musculoskeletal Association of Chartered Physiotherapists (MACP) to be a vehicle for Advanced Practice and the MACP to be rebranded.
I would not be surprised if this study was instrumental in NHSE’s decision to axe the portfolio route.
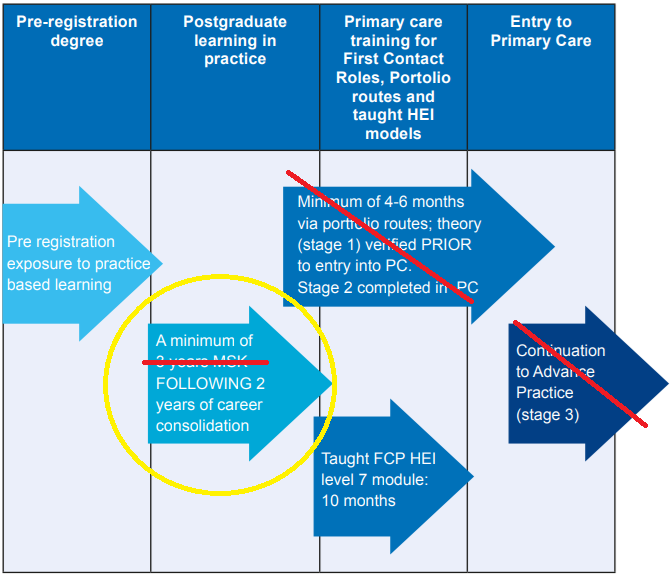
The Illustrative Roadmap in practice now:
My Experience On The Ground
Let’s unpack what’s happened from the lens of being on the ground. Out of the blue I heard the register to the Centre of Advancing Practice was being withdrawn. In addition, the portfolio route was closing within six months. FCP trainees needed to complete stage 2 by the end of April 2023, after which the 900 roadmap-trained supervisors were going to be as useful as a chocolate kettle. Or as the CSP more eloquently put it, ‘the ongoing role for roadmap supervisors is not entirely clear and may be disadvantaged by this decision’ [5].
LinkedIn posts turned from ‘what a great place I work at’ to a steady stream of ‘I’ve been roadmap signed off’. However, office chatter was about ‘what a waste of time and effort this portfolio has been’. A glum and negative reflection in hindsight. Perhaps appropriate given the NHSEs gut punch, its lack of national announcement, it's incredibly poor communication and the sheer amount of work involved in training.
Most disappointing was the abandonment of any form of formal recognition. The solution is to keep your sign off sheet and portfolio evidence on a USB stick. Don’t worry if you lose your USB stick or your computer corrupts. Don’t stress if your USB stick does not work on an NHS Trust computer when in an interview. It’s not like these sign off sheets can be doctored…right? Indeed, laugh/cry out loud. Other advice from the CSP was to speak to your local primary care training hub, sigh!
CSP Position, HEI Quality Assurances And Third Party FCP Providers
The CSP is in a hard place with this and their position is clear: ‘The changes being implemented now by NHSE WTE should lead to a more effective, better governed system of recognition using Higher Education Institutes’ (HEI) quality assurance processes, which will be easier for members to navigate’ [5].
The key word there is ‘should’. But check out the current course entry requirements for the FCP course at Bradford University. At the time of writing, it allows sports massage therapists and sport rehabilitators with up to three years’ experience to apply. The requirements are: ‘Usually, three years of post-registration experience, ideally in a musculoskeletal setting. Your ‘Learning Needs Analysis’ (LNA) will inform suitability rather than years of practice’ [6].
Seriously! So much for the quality assurance processes. The University of Essex entry requirements do not state any need for HCPC registration [7]. The University of Hertfordshire allows registered osteopaths [8]. A list of other UK universities without direct NHSE funding have questionable entry criteria and many do not need you to be a registered physiotherapist.
Paradoxically it appears some HEIs may have lowered the standards of recognition. One already mentioned receives funding for its FCP courses from NHSE. Again being real about this, HEIs need to make money and it appears to have a negative impact on our profession.
This brings me on to the free market and the worrying rise of FCP roles targeting clinicians with less than three years’ experience. For the FCP providers who think missing years can be made up by acquiring a post-grad Masters, think again.
Are we really showing our primary care colleagues good governance? Are we not mindful of the British Medical Association’s view on poor governance with respect to Physician Assistants? Did FCPs not experience collateral damage during the row over PAs [9]?
How is this better governance? How does this benefit Chartered physiotherapists? Does this protect the public? What is the purpose of a protected title unless you work in cardio, neuro or respiratory fields?
Lots of FCPs work for third party providers. Here the 100% reimbursable salary cake is cut and divided up between the Primary Care Network (PCN), the third company and what’s left is your salary. So I wonder how many open conversations have been had about your salary? In NHS Trusts pay is via the Agenda For Change contract so things are more transparent.
You probably know the third party provider names. LinkedIn is full of adverts. It’s a market reliant on the flow of money from the GP contract [10], specifically the Network Contract Directed Enhanced Service (DES Contract). The FCP role is described as an ‘additional role’ and referred to as the Additional Roles Reimbursement Scheme (ARRS). The ARRS budget is 100% reimbursable as I previously mentioned. Third company providers are a bit like recruitment agencies if you can forgive the clumsy comparison.
They offload PCN costs for payroll, recruitment onboarding, in-house supervision and development. Some providers have FCP leads with as little as 2-3 years experience in MSK. Many show value by meeting targets. Worryingly 78% of FCPs are either exhausted or at risk of exhaustion according to the first study of its kind [11]. The bulk of FCPs work with 20 minute appointment times and less than 5 hours non-clinical time per month. Outrageous!
So a PCN wants to recruit an FCP but is concerned about how to implement one. They mitigate its business risks by contracting a third company provider who perhaps works their FCP into exhaustion. Standards across companies vary. Questionable ones often have job adverts where 1-2 years experience is all that's needed. Or they recruit a MSc graduate with less than 3 years working experience. This is poor governance slapping you in the face.
Let’s be realistic here and state the obvious. For some companies the bottom line matters more than standards and fair pay. Think of it this way, if you were a PCN and/or third-party company, would you not be tempted to pay less? In five years’ time would these same companies be happy to pay even less and go along with the HEI-trained sport therapist?
Public protection and regulation
The HCPC is there to protect the public. They last commissioned a report in 2020 on the question about whether advanced practice should be regulated for public protection. They found no concerns or evidence it should [12]. Coincidentally the HCPC commissioned this research from Bradford University. I think it's reasonable to say a lot has changed since 2020 in the FCP landscape and I would like the HCPC to look at this again. Regulation of both enhanced and advanced practice seems a no brainer to me. The Nursing and Midwifery Council (NMC) agrees with the need to regulate advanced practice in nursing [13].
The provision and delivery of quality-focused workplace support is an essential component of the model curricula of enhanced practice [14]. It is crucial for the employer, professional, and for those who access services in safeguarding high-quality care and is set out as an expectation by the HCPC proficiency standards [14,15].
FCP sits in the enhanced practice domain which is prior to advanced practice, see Figure 1. An enhanced practice curriculum [16] has been produced to support the Enhanced Clinical Practitioner apprenticeships and CPD routes [17]. Recognising and formalising Enhanced Level Practice will drive cultural change and provide a positive impact on services. This is what the FCP Roadmap achieved.
Final Thoughts
I strongly believe the CSP have our backs, and they provided a clear statement ‘we strongly advocate that members who have already completed the roadmap should be recognised as such and not be disadvantaged by the new process’ [5].
Thousands of portfolio graduates who have no qualification/recognition. It's unfair and unjust for those who made all the right first impressions with our PCN colleagues and completed the roadmap in good faith. One could argue it has created a ‘better than you’ scenario. How do the PCN managers view these differences? How will these be viewed in five years time? Picture this, given all else is equal, if an employer is choosing between a certificate holder or a CERTIFICATELESS practitioner, who are they going to choose?
The Network Contract DES [10] which is the contract PCNs use when implementing ARRS funded services like FCP currently stipulates that FCPs must be HCPC regulated (see annex B of the contract). But how tight is this in law? and could that stipulation be removed?
The advanced centre will only be registering advanced practitioners and because embarking on an MSc for many of us is unaffordable, it creates inequality based on disposable income. Not many of us qualify for grants.
It's my strong opinion that to secure our reputation, our jobs, and future in primary care, we need NHSE, CSP, HEIs leaders to pick up the pieces of this roadmap and FCP governance. FCP can be an excellent and rewarding job. Its purpose aligns with government aims of improving the public's access to physiotherapy in primary care. It has been shown to reduce burden on GP services [18].
However, perhaps a commission is warranted for an end-to-end review of FCP training, qualifications, regulation, supervision and implementation of the workforce. If all stakeholders cannot come to an agreement around governance, then there is even more reason for the HCPC to regulate to protect the public.
References
Noblet, T., Heneghan, R, N., Hindle, J and Rushton, A. (2021) Accreditation of advanced clinical practice of musculoskeletal physiotherapy in England: a qualitative two-phase study to inform implementation. Physiotherapy 113 217–244.
First contact physiotherapy roadmap changes – what they mean for you
First Contact Practitioner (Musculoskeletal) PGCert - University of Bradford
First Contact Musculoskeletal Practice | University of Essex
Short Course - First Contact Practitioner Musculo-Skeletal FCP Stage 1 | Courses | Uni of Herts
The collateral damage caused by the row over physician associates | Comment | Health Service Journal
NHS England » Network Contract Directed Enhanced Service (DES)
https://doi.org/10.1002/msc.1752. Lewis Nozedar. Musculoskeletal Care. 2023;21:776–785. What is the prevalence of burnout amongst first contact physiotherapists working within primary care?
Advanced practice review - The Nursing and Midwifery Council
AHP enhanced practice | NHS England | Workforce, training and education
Allied Health Professions Enhanced Level Practice Schemas with Model Curricula
Mercer, C & Hensman-Crook, A (Volume 62, December 2022, 102623). Editorial. First Contact Practitioners- new opportunities for musculoskeletal expertise in Primary Care.Musculoskeletal Science and Practice










What a very well written piece. I have had my share of stresses with the FCP process as a supervisor during its roll out. The key stand out here, sadly, is the continued (and by the sound of it worsening) poor communication and transparency. I suspect it'll only come to light once there has been some higher profile serious incidents.
Thank you for this clear expression of the troubles facing the FCP community. Recognition is needed but I fear is low on the priority list.